The use of immune-mediated treatment of cancer is leading to dramatic improvements in patient outcome, but it also has new toxicity profiles, making it vital to recognize imaging manifestations of adverse effects, award-winning Spanish researchers have reported.
While standard antineoplastic therapy is associated with immunosuppression and infections, these new therapies induce overwhelming inflammation and autoimmunity, noted Sonia Lon Colvée and colleagues at Hospital Clínico Universitario San Carlos in Madrid. Most adverse events are mild or moderate, but severe and life-threatening complications requiring admission to the intensive care unit can also occur.
"This situation makes the role of the radiologist key when it comes to optimizing treatment individually for each patient, taking into account the risks and benefits of the different therapies," they stated.
As part of a new analysis, the team selected a group of patients who underwent immunotherapy treatment at San Carlos from 2018 to 2022. They correlated the clinical features they presented with during emergency episodes or routine follow-up with CT, PET/CT and/or MRI. Adverse effects were classified according to organ-specificity findings, the timing in their development after starting treatment, and the type of immunotherapeutic agents.
Complications usually occur in the first three months of onset and get resolved in about two to three months. The main risk factors are a history of autoimmunity and chronic infections, stage III-IV kidney disease, and combined therapies (PD-1 + CTLA-4). Also, complications are more common in men, and the use of pretreatment corticosteroids is a protective factor, they noted.
Immune-related adverse effects occur in cases of hypophysitis, synovitis, enteritis, different types of pneumonitis, and colitis.
Patients with pneumonitis
At San Carlos, cryptogenic organizing pneumonia is the most prevalent condition, "consisting of a discrete patchy or confluent consolidation ± air bronchograms predominantly in a peripheral or subpleural distribution. Ground glass opacities are also observed in some cases, seen as discrete focal areas of increased attenuation with preserved bronchovascular markings."
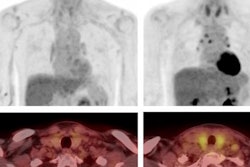
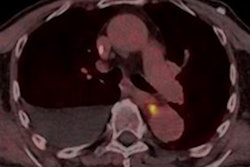
In a patient who had received two months of treatment with pembrolizumab, a PET/CT study showed patchy peripheral consolidations, and the diagnosis was inflammatory pneumonitis. This patient died two months later due to an infectious pneumonia.
There is another rare lung condition called sarcoid reaction, the researchers explained. It is characterized by bilateral and symmetric hilar and mediastinal lymphadenopathy of new appearance +/- alterations in the parenchyma without infection and with evidence of response at other levels.
"It is more common in melanoma cases treated with anti-CTLA-4," they noted. "There was a patient in our center who developed a sarcoid reaction after five months of being treated with pembrolizumab. Treatment was changed to dabrafenib and trametinib. CT imaging findings disappeared a year later."
Keep aware of hypophysitis
Hypophysitis, or inflammation of the anterior lobe of the pituitary gland, presents with headache, fatigue, dizziness, and memory impairment. Most patients have anterior pituitary hormone deficiencies at presentation, and hormone replacement should be instituted soon after diagnosis, Lon Colvée and colleagues pointed out. It typically presents six to 12 weeks after initiation of anti-CTLA-4 therapy.
"MRI findings include an enlarged pituitary gland and stalk with variable heterogeneous or homogeneous enhancement," they continued. "Treatment is a form of high-dose glucocorticoids and temporary or complete cessation of immune checkpoint inhibitor (ICI) therapy."
Resolution of pituitary findings on MRI, along with resolution of clinical symptoms, is often noted during immune-related hypophysitis. MRI plays an important role for both detection and monitoring of this condition.
Dealing with colitis and enteritis
Colitis and enteritis are the most frequent severe complications, and they can lead to a high mortality rate if treatment with corticosteroids is delayed, the authors wrote. Typical clinical features are diarrhea, abdominal pain, and fever.
"Imaging can depict signs of colitis/enteritis on CT as well as its complications, such as bowel perforation, obstruction and toxic megacolon," they noted. "Radiological findings are diffuse wall thickening, mucosal enhancement, submucosal edema, and fat stranding."
In cases of colitis, the more common pattern is diffuse colitis with mild bowel wall thickening, mesenteric vessel engorgement, and a fluid-filled colonic distension. This was the case of a patient at San Carlos who was treated for lung cancer with pembrolizumab and six months later started with abdominal pain and diarrhea. An autoimmune episode was diagnosed.
The other type consists of a segmental colitis associated with diverticulosis. It affects a segment with preexisting diverticulosis with superimposed circumferential bowel wall thickening and mesenteric vessel engorgement, the authors wrote.
Pancreatitis is a rare adverse event, and imaging is indistinguishable from pancreatitis of any other etiology. Pancreatitis has also been observed in association with anti-CTLA-4-induced enterocolitis. Hepatitis is typically asymptomatic, and it is diagnosed as an elevation of transaminase on routine blood tests, they explained.
To view the entire e-poster, go to the EPOS section of the ESR website. The co-authors of the e-poster were Maria Guerrero Martin, Álvaro Rueda De Eusebio, Sara Gómez Peña, Carmen Polidura Arruga, Natividad Gomez Ruiz, Paula Hernandez Mateo, and Irene Martin Lores. The group received a cum laude award for their work presented at ECR 2023.