For women with symptomatic fibroids, uterine artery embolization (UAE) is one of the main treatment options alongside surgical procedures, endometrial ablation, and medical management, a working group that includes the U.K. Royal College of Radiologists (RCR) has noted in new guidelines.
The group's recommendations are freely available for download on the RCR's website, and these are the key points:
- The early and medium-term (to five years) results of UAE are good. It is as effective as surgery for symptom control, with the caveat that about one-third of women will require a second intervention by five years.
- The evidence for fertility and pregnancy outcomes after UAE and after myomectomy is poor. Similarly, there is no robust evidence comparing UAE or myomectomy for these outcomes. "Currently it is impossible to make an evidence-based recommendation about treatment (UAE or myomectomy) for women with fibroids who wish to maintain their fertility. Treatments for fibroids in women of childbearing age who wish, or might wish, to become pregnant in the future should be offered only after fully informed discussion," the working group wrote.
- The procedure is contraindicated in women who have evidence of current or recent pelvic infection, who are pregnant, who are not prepared to accept the small risk hysterectomy may be required in the event of complication, or in whom there is significant doubt about the diagnosis of benign pathology.
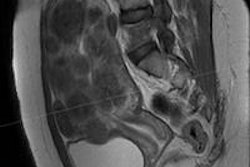
- Patients should be selected and assessed by a multidisciplinary team including a gynecologist and an interventional radiologist. Direct referral from primary care to an interventional radiologist is acceptable, although local governance arrangements should ensure gynecology input into the management of patients referred in this way. Accurate pretreatment diagnosis with MRI is recommended.
- The procedure should only be undertaken by radiologists with established competence in embolization techniques and who have undergone appropriate training.
- The responsibilities of both the gynecologist and radiologist for the care of the patient should be established prior to treatment and be set out in a relevant hospital protocol. The patient must be under a named responsible consultant at all times -- this could be a radiologist or a gynecologist (or both). Comprehensive follow-up protocols should be established. This should include contact telephone numbers for advice after discharge from hospital.
The new guidelines (Clinical recommendations on the use of uterine artery embolization in the management of fibroids, Third edition) are intended to provide information for patients interested in undergoing UAE and guidelines for clinicians involved in their care, and they replace earlier versions. In the U.K., the recommendations are intended for both the National Health Service (NHS) and private sector, the working group wrote.
Arterial embolization has been used during the last three decades as a method of treating gynecological hemorrhage in a variety of clinical situations, including postpartum hemorrhage, bleeding after caesarean section, and bleeding following gynecological surgery. The technique was subsequently used for the management of arteriovenous malformations of the genital tract and in gestational trophoblastic disease.
In 2000, a Joint Working Party of the Royal College of Obstetricians and Gynecologists and the RCR was established to issue guidance on UAE -- a procedure which at that time was in its infancy with fewer than 7,000 cases undertaken worldwide. Since the publication of the guidance, the procedure has become well-established and more than 100,000 cases have now been performed worldwide. The evidence from national registries and randomized trials has demonstrated that UAE has good short- and medium-term success rates with acceptable morbidity and very low mortality.
Evidence base
The working group based its recommendations on a literature review and includes a recent Cochrane review (2012) that offers the most succinct description of the current evidence for UAE. The procedure has an overall patient satisfaction rate similar to hysterectomy and myomectomy while offering an advantage with regard to a shorter hospital stay and a quicker return to routine activities.
UAE, however, is also associated with a higher rate of minor complications and an increased likelihood of requiring surgical intervention within two to five years of the initial procedure, the Cochrane review acknowledged. There is limited evidence suggesting that myomectomy may be associated with better fertility outcomes than UAE, but more research is needed.
The radiologist's responsibility
When deciding how to treat fibroids, a discussion between the patient and gynecologist -- or general practitioner with gynecology experience, accreditation, and competence -- is necessary. After the woman has been referred, the decision to treat, work up, preprocedural imaging, and the technical details of the procedure are the responsibility of the radiologist. For patients referred direct from primary care, the radiologist should ensure gynecology input is obtained. Postprocedural care may be gynecology-led, radiology-led, or a combination.
"The most important element in the continuing care of the patient is that they should have rapid access to follow-up to allay any anxieties relating to expected sequelae and to act immediately if there is any question of the development of a problem," the working group wrote. "Models may be gynecology-led or radiology-led although it is anticipated, given the current service structure in the NHS, that most patients with complications will be admitted under the care of a gynecologist. In any event, close communication is vital."
Clinical radiologists may take principal medical responsibility for the care of a patient for part or all of the hospital stay on the same basis as any other registered medical practitioners, the working group noted. That is, provided the radiologist's skills, training, and available facilities are sufficient to ensure appropriate care until responsibility is reassumed by the referring medical practitioner.
"Where radiologists are working in a hospital without a gynecological unit, agreed procedures for communication between clinicians allowing rapid recourse to an appropriate specialist are essential," the working group wrote.
In terms of follow-up, at least one follow-up appointment at six months after the procedure should be offered, although details of protocols vary. Telephone follow-up is acceptable as long as clinic follow-up is available if requested or necessary. Imaging is mandatory if symptoms persist or recur, they added.
More research is needed
While the safety and efficacy of UAE in the short- and medium-term has been proved, the group noted that more research is needed on the following:
- Comparing UAE with myomectomy for symptom relief, fertility, and pregnancy outcomes and ovarian reserve
- Optimization of embolization technique, including identification of the ideal embolic agent and embolic endpoint
- Efficacy of prophylactic antibiotics
- Comparison with other nonsurgical techniques, such as MR-focused ultrasound therapy
- Stratification of results by fibroid position, size, and number
- Screening for pretreatment infection
- Effects on psychosexual function