Molecular imaging (MI) is enhancing assessment of therapy response and facilitating risk-adapted, personalized therapy in malignancies. Moreover, research on exploiting the specific molecular features of tumors and their microenvironment can translate into better future clinical care, delegates learned at the 2013 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) congress.
"MI has become synonymous with FDG-PET, which has impacted patient care in numerous abdominal malignancies; however, on the horizon are new MI applications," noted Dr. Ur Metser, an associate professor in the department of medical imaging and head of the molecular imaging division at the University of Toronto. "Although we, as radiologists, are accustomed to look at morphological changes to identify disease process, the underlying biology represents a new arena for most of us."
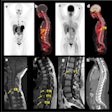
 Patient with small-bowel carcinoid shows expression of somatostatin receptors in primary tumor and in liver deposits. The radiotracer Ga-68-DOTA NOC is specific for somatostatic receptors 2, 3, and 5. Maximum intensity projection (MIP) image shows focal uptake in liver and in right upper quadrant (primary tumor in small bowel). All images courtesy of Dr. Ur Metser.
Patient with small-bowel carcinoid shows expression of somatostatin receptors in primary tumor and in liver deposits. The radiotracer Ga-68-DOTA NOC is specific for somatostatic receptors 2, 3, and 5. Maximum intensity projection (MIP) image shows focal uptake in liver and in right upper quadrant (primary tumor in small bowel). All images courtesy of Dr. Ur Metser.Emerging MI techniques directly or indirectly monitor and record the spatiotemporal distribution of molecular or cellular processes for biochemical, biologic, diagnostic, or therapeutic applications, he explained in a practical e-poster presented at the ESGAR meeting in Barcelona. MI probes the molecular abnormalities that are the basis of disease rather than the end effects of these alterations.
"Traditionally, a distinction has been made between anatomic imaging, such as CT or MR and physiologic imaging, nuclear medicine. However, this simple distinction is increasingly becoming blurred by functional information provided by CT and MR and by fusion technologies such as PET/CT and now PET/MR," he stated. "Most, but not all, functional imaging is also MI. For example, blood-oxygen dependent or BOLD imaging on MR is an example of functional imaging which does not address a biologic event on a molecular scale."
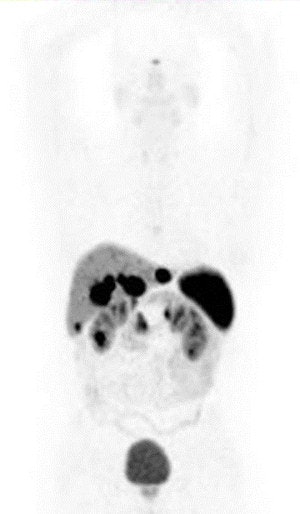
FDG-PET can accurately identify residual viable disease in patients with high-grade lymphoma with residual masses after completion of therapy. With MI, it is also possible to predict response to therapy early in the course of treatment.
In Hodgkin's lymphoma and aggressive B-cell non-Hodgkin's lymphoma, PET performed after only two or three cycles of chemotherapy can provide valuable prognostic information, helping to identify chemoresistant tumors early on and facilitate individualized risk-adapted therapy, according to Metser.
Prior prospective trials have shown there is a high association between negative early interim PET (after two cycles of chemotherapy) and progression free and overall survival. Nearly all patients with advanced stage Hodgkin's lymphoma that have residual uptake of FDG at tumor sites after two cycles of chemotherapy will relapse within two years, compared with only 1.6% to 13% of patients that have a negative early interim PET scan, he continued.
"An early PET result may offer a window into the chemosensitivity of the tumor. Chemotherapy kills tumor by first-order kinetics: A given dose kills the same fraction of cells (not same number) regardless of tumor size," Metser explained. "It should be stressed that a negative interim PET does not mean lack of viable disease, but rather that tumor is chemosensitive and patient has a very high likelihood of being disease-free at the end of the current course of therapy."
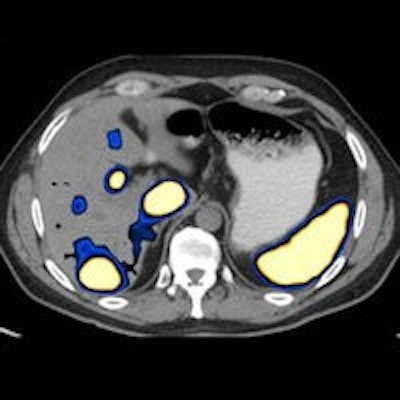
 Same patient. Axial images (CT on left, PET in middle, fused PET/CT on right) show primary tumor in small bowel (above) and multiple liver metastases expressing somatostatin receptors (below).
Same patient. Axial images (CT on left, PET in middle, fused PET/CT on right) show primary tumor in small bowel (above) and multiple liver metastases expressing somatostatin receptors (below).
To tailor therapy according to risk, one option is to decrease the number of cycles of chemotherapy or omit radiation (and decrease toxicity), while another is to escalate therapy if the interim PET scan is positive (and potentially increase toxicity), he suggested. Multiple prospective trials are underway to assess this topic.
It is also feasible to image receptors and determine receptor density -- a concept that has existed for decades, one common example being somatostatin receptor imaging for neuroendocrine tumors (NETs).
 Patient with non-Hodgkin's lymphoma. Baseline PET (MIP image on left) shows involvement of nodes above and below diaphragm and spleen (arrows). After two cycles of chemotherapy, no residual abnormal uptake is visualized, indicating favorable early response to therapy.
Patient with non-Hodgkin's lymphoma. Baseline PET (MIP image on left) shows involvement of nodes above and below diaphragm and spleen (arrows). After two cycles of chemotherapy, no residual abnormal uptake is visualized, indicating favorable early response to therapy."We know that tumor receptors play an important role in carcinogenesis and tumor growth. Knowledge of receptor expression is key for therapy directed at tumor receptors. We can estimate receptor density with molecular imaging probes," Metser noted. "Our experience has taught us that expression of receptors may be heterogeneous within tumor and even may also vary between primary tumor and metastatic deposits."
Although there are conflicting initial reports, some investigators suggest PET with gallium-68 (Ga-68)-labeled somatostatin analogs may contribute to the early prediction of treatment outcome in patients with well-differentiated NETs undergoing peptide receptor radionuclide treatment. Larger scale trials to clarify the role of PET in assessing response to therapy are pending, he stated.
Hypoxia can be imaged with MI probes, specifically with various nitroimidazole compounds. These compounds contain a bioreductive molecule that accepts a single electron, leading to free radical metabolites that are further reduced and bound to cell constituents under hypoxic conditions. To simplify things, these compounds need hypoxia to bind to cells and therefore they accumulate in hypoxic cells, one such hypoxia agent being FAZA (F-18-labeled fluoroazomycin arabinoside), Metser concluded.