Combining CT perfusion (CTP) scans with CT angiography (CTA) can improve the diagnosis of coronary artery disease in stent patients, visualizing stenotic vessel segments that CTA alone is hard-pressed to characterize, German researchers reported in the Journal of the American College of Cardiology.
The study of almost 100 patients with suspected in-stent restenosis found that combined CTA/CTP was significantly more accurate than 320-detector-row CTA alone at both the per-patient and per-vessel levels, mostly by visualizing vessels that were nondiagnostic at CTA. The combined test was also more accurate for the diagnosis of CTA alone, offering the potential of speeding diagnosis while eliminating unnecessary invasive angiography exams.
"The noninvasive detection of coronary stenosis in patients with stents by CTA alone is limited, and the combination of CTA and CTP has the potential to improve diagnostic performance by adding functional information that may also be relevant to the decision whether or not to perform revascularization in symptomatic patients," wrote Drs. Matthias Rief, Elke Zimmermann, and colleagues from the Charité Hospital in Berlin, along with colleagues from Eberhard Karls University in Tübingen and University Hospital of Friedrich-Schiller University in Jena (JACC, 18 June 2013).
Tough calls, made too often
Stent implantation has become an increasingly common procedure owing to its success in eliminating angina symptoms better than medical therapy, the authors wrote. Stents are now used in 90% of all percutaneous interventions, and total more than half a million procedures each year in the U.S. and more than 850,000 in Europe. But stent assessment has been and remains a big challenge for cardiac CTA, particularly now that it is being used in smaller and smaller vessels that are difficult to visualize. The examination is burdened by artifacts, and when used alone can't gauge the functional significance of lesions.
In an accompanying editorial, Dr. Andrew Arai, a senior investigator in the Advanced Cardiovascular Imaging Group at the U.S. National Institutes of Health in Bethesda, Maryland, noted that coronary CTA is not recommended in patients with stents because so many exams are nondiagnostic "mainly due to artifacts resulting from the metallic material of stent struts and coronary artery motion." Moreover, "high and irregular heart rates enhance artifacts caused by metal stents," and "make the exams difficult to read," he wrote. As for a key alternative exam, MRI is degraded by signal loss within the stent (JACC, 18 June 2013).
The study, known as Coronary Artery Stent Evaluation with 320-row CT (CARS-320), aimed to prospectively evaluate CTA's ability to detect in-stent restenosis compared with quantitative coronary angiography (QCA) as the reference standard. The wide-open recruitment criteria included all patients and stents regardless of type, size, or number of stents and time since implantation, even if an exam or a vessel segment was nondiagnostic. Thus, the study's population, though all were in sinus rhythm, tackles a set of patients that challenges CTA as it does in daily clinical use.
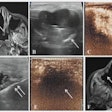
Blooming artifact from coronary stents can make it difficult to accurately assess for in-stent restenosis and reduces the diagnostic accuracy of CTA alone. Patients with severe coronary disease often have heavily calcified coronary arteries that can also compromise the ability to accurately predict the presence or severity of native coronary stenoses.
CTA and CTP were performed in 91 consecutive patients who had from one to 10 stents (average of 2.5 ± 1.8) with diameters of 3.0 ± 0.5 mm. Beta-blockers were given to 84% of patients prior to contrast administration and prospectively gated CTA imaging on a 320-detector-row CT scanner (Aquilion One, Toshiba Medical Systems) at 120 kV and tube current adjusted to body mass index (BMI).
Immediately after CTA, CTP was performed after nitroglycerin administration and four minutes after a second contrast injection, with images acquired and reconstructed using 0.5-mm slices.
"Whenever a coronary stent or vessel was nondiagnostic on CTA, adenosine stress CTP in the corresponding myocardial territory was read for combined CTA/CTP exam," Rief and colleagues noted.
QCA was performed by a separate investigator who was blinded to the CT results and evaluated at least two orthogonal projections, measuring the highest degree of narrowing according to 16-segment American Heart Association criteria.
Better together
Combined coronary CTA and myocardial CTP outperformed CTA alone in detecting coronary in-stent restenosis and coronary artery disease, with significantly more patients (22%) deemed nondiagnostic at CTA compared with CTA plus CTP (1% p < 0.001). At CTA alone three-fourths of the nondiagnostic exams were due to metallic artifacts versus one-fourth for cardiac motion.
In addition, the diagnostic accuracy of CTA/CTP for stents (87%; 95% confidence interval [CI]: 78% to 93%) was significantly higher than that of CTA alone (71%; CI: 61% to 80%; p < 0.001) per patient, mainly due to the reduction in nondiagnostic exams.
The diagnosis of coronary artery disease was boosted by the addition of CTP (p < 0.001). And interestingly, CTA/CTP had a significantly lower effective radiation dose (7.9 mSv ± 2.8 mSv) compared with angiography (9.5 mSv ± 5.1 mSv; p = 0.005).
Combined CTA/CTP demonstrated 87% accuracy for detection of in-stent restenosis and 86% accuracy for CAD per patient, "which is the most relevant level and indicates robust diagnostic performance," Rief and colleagues wrote, whereas CTA alone showed only 71% diagnostic accuracy for in-stent restenosis diagnosis and 81% for CAD.
"CTP primarily uses visual analysis supplemented by assessment of absolute densities, as well as transmural density differences," the authors wrote. "In other studies, this approach has provided incremental diagnostic power over CTA alone in suspected or known CAD."
This study makes an intraindividual comparison using 320-detector-row CT, and shows that both in-stent restenosis and CAD diagnosis is improved by both exams, they added.
Other noninvasive imaging modalities, including myocardial SPECT, cardiac MRI, and stress echocardiography, and CTP by itself alone may not be accurate enough to reliably rule out in-stent restenosis. CTA/CTP was also much more accurate than stress tests.
"Our results confirm the increased nondiagnostic rate of CTA in stents with small (< 3 mm) inner diameters," the authors wrote. "Importantly, CTP was not affected by such challenging stent characteristics."
"CTA provides accurate anatomic localization of stenoses, stents, heavily calcified coronary arteries, and the myocardium served by the coronary arteries affected by these apparent or possible stenoses," Arai added in his editorial. "Stress CTP perfusion then provides a physiological assessment of physiological significance of the stenoses."As for limitations, the CT scans were preceded by coronary artery calcium scans, which limit the territory and the dose for subsequent CTA and CTP exams, the authors wrote.
As for competing exams, Arai noted the utility and increasing interest in CT fractional flow reserve exams, which require no additional radiation exposure, and noted that quantitative PET perfusion and quantitative stress MRI could "theoretically" measure myocardial perfusion reserve if that test pans out in future studies.
The trial was funded by Italian contrast developer Bracco Imaging.