Do not fear teleradiology, asserts Dr. Philip Gishen, the respected radiologist who restored calm and order at two of London's top hospitals after turbulent times. He has nurtured a special interest in teleradiology, and is convinced it can deliver high standards and won't take away a radiologist's job.
Gishen has never been afraid of change, in fact he positively welcomes it. It was his radical shake up that transformed the radiology services at Hammersmith and Charing Cross Hospitals in the early 2000s. He continues to embrace the changes the digital world brings to radiology, spending at least one day per week as clinical director at Radiology Reporting Online (RRO), a teleradiology company strategically situated opposite University College Hospital, London.
 Dr. Philip Gishen is the clinical director at Radiology Reporting Online, a teleradiology company.
Dr. Philip Gishen is the clinical director at Radiology Reporting Online, a teleradiology company.Arguably, teleradiology's journey from concept to practice has proven to be a one-way street. Over the past decade, radiology entered the digital age, driven by the growth and progressive standardization of Internet and broadband facilities across hospital trusts. Teleradiology, which entails the digital transfer of images to reporting radiologists, presented the obvious answer to relieving radiologists from a long night on call and an even longer following day at work.
"A radiologist on call at a district general hospital will be called between three to 10 times in a night, and would be expected to work a full day the next day," Gishen said. "This might be sustainable for a few years, but over a career this is not feasible, so we needed to find a solution to this."
He pointed out that radiology needed people available at night. "If we had 10 or 20 hospitals each with four cases in a night, then one or two radiologists could manage all these cases. This is how teleradiology came about."
A history of implementing change
Gishen's appetite for change happened long before teleradiology arrived. Born and educated in South Africa, Gishen came to the U.K. to take up a post at Kings College Hospital, London in 1977, where he served as a consultant for 24 years. Then in 2001, Hammersmith and Charing Cross Hospitals asked him to join them in the hope he would rejuvenate the radiology departments.
A huge number of changes took place under Gishen's tenure as head of department. Hammersmith had a PACS-enabled department, but Charing Cross did not. Gishen introduced PACS and voice recognition to the latter. "Also, instead of using the department's valuable work stations for a couple of hours a day we organized schedules so it was in use constantly. We improved on call so the right and most relevant people were on call at any one time."
Staffing balance was addressed, reflecting emerging trends in radiology such as a need for specialists in musculoskeletal (MSK) or neuroradiology. "Timetables needed to be corrected to hourly working rather than sessions. This extended department working hours without increasing consultant staff levels. Effectively, radiologists were given more control of their working hours," Gishen said. The efficiency changes seen at Hammersmith and Charing Cross had primed Gishen to enthusiastically embrace teleradiology and the workflow advantages it offered.
"The big change in imaging was the shift from analogue to digital images. We now had digital images that could move anywhere. PACS was a massive change," he emphasized.
Naturally, Gishen took the bull by the horns and embraced all that teleradiology had to offer. RRO has a team of 40 teleradiologists, all of whom are General Medical Council (GMC) qualified, including the Australian-based team who report the U.K. emergency overnight work.
Fear unfounded
Unsurprisingly, teleradiology is not without its critics, mainly radiologists who fear that it will eventually dilute their responsibilities and undermine their jobs, but Gishen explained why he believed these concerns should be seen in the broader context.
"Teleradiology brings consistency and continuity of contact that the old, on-call system did not. Previously, if a radiology department had 20 doctors, then each radiologist might be on call two nights per month. This set up meant that clinicians were in contact with different radiologists each night. Now they get the same two or three radiologists each night."
Addressing the fears for their jobs, Gishen added there was no doubt that radiologists would continue to have defined and indispensible roles in departments. "Particularly in interventional radiology -- blocked structures such as ureters, blood vessels, and leaking arteries is all interventional radiology work now -- that is not going to be replaced by teleradiology."
In the past, there has also been some concern about teleradiology companies contracting readers and reporters in countries where certain standards might not routinely meet those adhered to in the U.K. According to Gishen, this practice is on the decline, if it happens at all today.
To allay these fears, RRO has a bespoke program that double reads 10% of cases. "All images are scored and shared with staff and any mistakes are fed back. Cases that went well and cases where reading didn't go so well are shown at regular Clinical Governance Meetings."
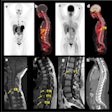
But Gishen acknowledges there are some valid concerns about teleradiology, notably that it is not suitable for everyone. In particular, he pointed out specialist radiologists might find it challenging reporting urgent overnight work, typically more suited to general radiologists. "For example, an MSK radiologist wouldn't be expected to know about an intracerebral bleed. Pediatrics is very specialized as well."
In Australia, RRO have two permanent radiologists with another six supporting them in shifts. The majority of cases at night are not specialist but the day cases can be, so RRO has specialist radiologists in the U.K. to meet this demand, such as in neurology or CT colonography. "In particular, we are finding a requirement for MSK radiologists due to a rapidly growing workload in this field," Gishen said.
Ultimately, like most interventions and practices in medicine, teleradiology needs to accumulate a substantial body of evidence documenting its effects on patient-related outcomes to encourage more widespread use. Rhiannon Williams, managing director at RRO, highlights this: "There is a pressing need to explore how radiology, including teleradiology, accelerates turnaround and patient outcomes and whether it makes a difference to length of stay in hospital."
"The key problem here is that, for the majority of work, there is no [National Health Service] tariff for radiology," she added. "A tariff would make it easier to understand the price and value of an MSK scan, for example, with a hip operation pathway. This is especially true in the context of the upcoming outcomes framework."
Reporting all cases -- don't cut corners
Gishen recognizes teleradiology is a cornerstone of change in NHS radiology services, but he also acknowledges it is only one piece of the jigsaw. Without laying the blame at any one hospital's door, his major bugbear relates to the incompleteness of reporting and the cutting of corners.
"It is the job of the radiologists to make sure every single image has an associated report," he stressed, noting that radiologists should be mindful of unreported images raising real fears amongst the patient population.
"I think radiologists should report all the cases. I think this is a requirement and it is unacceptable that a computer does pseudo-reports," he added.
In addition to ensuring that all reports are read, Gishen wants to see revision to the "red dot" system, which entails flagging up an abnormality to the relevant clinician. That is currently the responsibility of the radiologist. "I believe the system should be different to this."
Currently, if any particular clinician is sending a case to imaging then that clinician has the responsibility to read the report, acknowledge on the computer that this has been done, and tick a box that says he has understood the report. If the clinician does not do this, then the radiologist should be alerted to discuss the case.
"There's a lot of tightening up to be done. So for example, if the patient has had a hacking cough for months and his report is clear then this information is vital for the patient's peace of mind and well being. All reports are important and should be read by the referring clinician," Gishen noted.
Clearly, Gishen's dedication to clinical work is paralleled by his ability to implement organizational change. Much relates to workflow practices that require changing attitudes and habits, but even more relates to optimizing use of the technology available. Whichever way you cut it, he noted there was no escaping the 24/7 cultural revolution in radiology.
"Digitalization has happened and has changed everything," he said. "Likewise, the equipment too changes everything. These days we could have 2,000 slices of the abdomen, which can be reconstructed in so many directions. We no longer look at static images but scroll. It's all evolving so quickly."
But even Gishen looks ahead to a time beyond teleradiology. He noted that computer aided diagnosis (CAD) could affect future practice. Comparing it to pathology, where a computer reads results of hemoglobin, he said CAD was a trend to watch for. "When this happens there will be fewer teleradiology requirements."
In a comment apt for someone running an around-the-clock reporting service, Gishen reflected on how time does not stand still. "When I went into radiology, ultrasound was black and white dots and hardly discernable. I thought people are reaching conclusions without good reason. How it has blossomed since."