Thanks to its ability to improve the conspicuity of focal lung disease, bone suppression image processing can significantly improve radiologists' accuracy in identifying focal pneumonia on chest radiographs, according to new research published online on 5 July by European Radiology.
In a retrospective observer study, a group from the University of Chicago found that the mean area under the receiver operating characteristic (ROC) curve for the eight radiologists participating in the study increased from 0.844 with standard images to 0.880 with the addition of bone suppression. The difference was statistically significant (p<0.001).
"While the degree of improvement might seem relatively small in this study, it should be noted that experienced radiologists can readily detect all but the most subtle findings in the context of a focused observer test such as this, whereas in clinical practice, more obvious findings are commonly overlooked," wrote a research team led by Dr. Feng Li, from the department of radiology. "On the basis of these results we believe that [bone suppression imaging], by improving the conspicuity of focal disease, will likely help radiologists to avoid such oversight errors."
Bone-suppression techniques have been shown to improve diagnostic accuracy in detecting lung nodules, but the researchers sought in their current study to evaluate the software's impact on radiologists' performance for detecting focal pneumonia.
Two radiologists who did not participate in the observer study selected 36 patients (19 men and 17 women with a mean age of 52) with 46 focal pneumonias from a radiology department teaching file produced from clinical cases at the University of Chicago Medical Center from January 2004 to March 2010. Cases were chosen due to the presence of unequivocal but subtle pneumonia.
The 46 pneumonias were present on 25 standard posteroanterior (PA) and 11 portable anteroposterior (AP) chest x-rays; the mean diameter for the focal opacities ranged from 12 to 60 mm with a mean of 28 mm. The researchers also included 20 control subjects without focal pneumonia on 15 PA and five portable AP chest x-rays.
Bone suppression imaging software (SoftView version 2.2, Riverain Technologies) was applied to the resulting 56 chest x-rays. Eight radiologists, including six attending radiologists with a mean experience of 12 years in reading chest x-rays, and two radiology residents, were asked to provide their confidence level for the presence of a focal opacity compatible for pneumonia for each lung.
The images were read first without bone-suppression imaging and then with the addition of the processed images. None of the observers had experience with reading bone-suppression images before.
The mean area under the ROC curve for the eight radiologists participating in the study increased from 0.844 with standard images to 0.880 with the addition of bone suppression.
"Focal pneumonias were frequently difficult to detect on the standard [chest x-rays] but were relatively more conspicuous, and therefore easier to detect on the [bone-suppression imaging] images," the authors wrote.
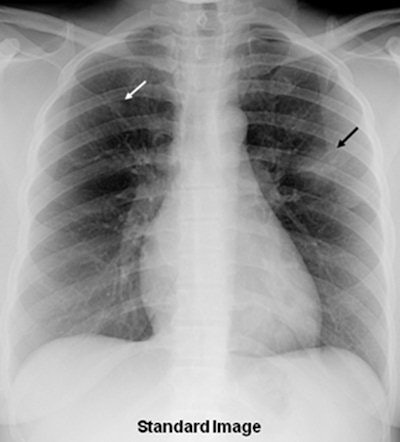
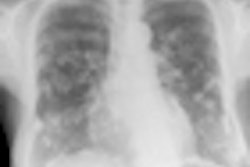
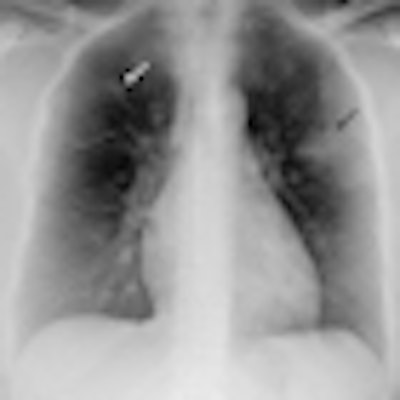
 A 36-year-old woman with focal pneumonia. Top: Portable chest radiograph shows focal airspace opacity in left upper lobe and a very small nodule in right upper lobe (arrows). Above: Bone suppression image shows these airspace opacities more clearly. Below: Coronal reconstruction from CT scan performed five days later. The right opacity had resolved and the left opacity had decreased on the follow-up CT. All images courtesy of Dr. Feng Li.
A 36-year-old woman with focal pneumonia. Top: Portable chest radiograph shows focal airspace opacity in left upper lobe and a very small nodule in right upper lobe (arrows). Above: Bone suppression image shows these airspace opacities more clearly. Below: Coronal reconstruction from CT scan performed five days later. The right opacity had resolved and the left opacity had decreased on the follow-up CT. All images courtesy of Dr. Feng Li.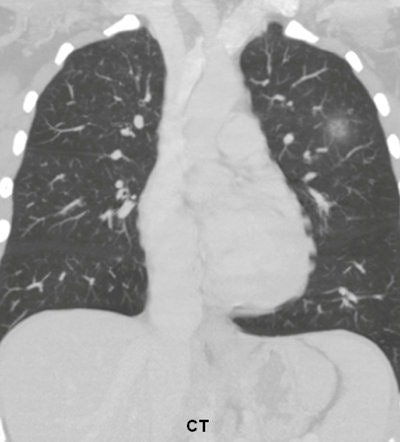
In further analysis of the data, the six attending radiologists experienced an increase in the mean value for the area under the curve from 0.865 to 0.900 with the addition of bone-suppression images (p = 0.001). Because there were only two radiology residents in the study, there was insufficient data for separate analysis of radiology residents as a group, according to the authors.
The researchers found the mean area under the curve improved significantly for the 40 PA chest x-rays from 0.850 with standard x-rays alone to 0.892 with the addition of bone-suppression images (p<0.001). They did not find a significant difference using just the 16 AP chest x-rays; mean area under the curve increased only slightly from 0.860 to 0.867 by adding bone-suppression images (p = 0.54) in this group.
The researchers did acknowledge several limitations of the study, including its retrospective design, the inability to extract meaningful results for radiology residents as a group, and the lack of use of dual-energy subtraction images.
"Nonetheless, the results described here suggest that use of bone suppression images in combination with standard [chest x-rays] can improve the detection of focal pneumonia compared with the use of standard [chest x-rays] alone," the authors concluded.
In the future, the researchers will study the performance of radiologists using SoftView in the detection of other lung abnormalities, they said.
|
Study disclosures The research was supported in part by a research grant from Riverain Technologies. One of the study's co-authors is a shareholder of Hologic/R2 Technology and also serves as a consultant for Riverain. Other co-authors receive royalties through the University of Chicago for computer-aided detection (CAD) technologies developed at the university that have been licensed to R2 (now Hologic), Deus Technologies, Riverain, Mitsubishi Space Software, Median Technologies, GE, and Toshiba. |